Do you have a problem with your mitral valve? Here are the symptoms to watch for.
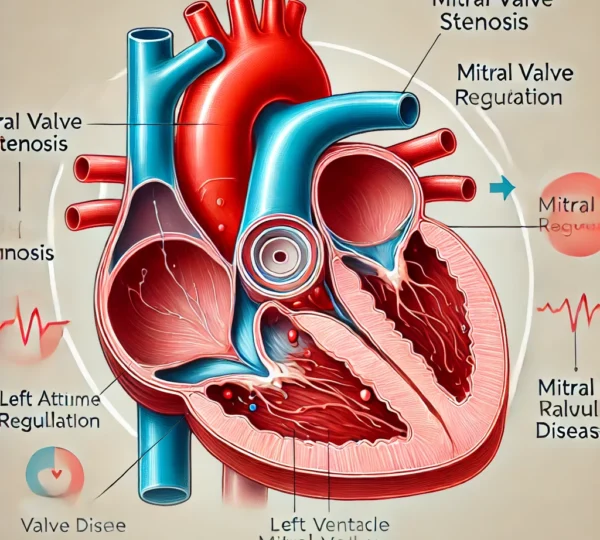
Mitral valve disease is a condition that affects one of the four main heart valves, the mitral valve. This valve plays a crucial role in controlling blood flow between the heart’s left atrium and left ventricle. When it isn’t working properly, it can lead to various complications, including heart failure, due to disrupted blood flow. Understanding mitral valve disease, its types, symptoms, and treatment options can help individuals recognize early signs and seek appropriate care.
Types of Mitral Valve Disease:
Mitral valve disease can manifest in different forms, primarily mitral valve stenosis and mitral valve regurgitation:
- Mitral Valve Stenosis: This occurs when the mitral valve becomes narrow, which restricts blood flow from the left atrium to the left ventricle. As a result, the heart has to work harder to pump blood through the narrowed valve, leading to increased pressure in the heart and lungs.
- Mitral Valve Regurgitation: This form involves a leaky mitral valve, causing blood to flow backward into the left atrium instead of moving forward into the left ventricle. Over time, this can enlarge the heart chambers and weaken the heart, potentially leading to heart failure if not treated.
Causes of Mitral Valve Disease:
Mitral valve disease can develop due to several underlying factors, including:
- Rheumatic Fever: A complication of untreated strep throat, rheumatic fever can damage the mitral valve over time, leading to scar tissue and impaired function.
- Congenital Heart Defects: Some people are born with abnormalities in the mitral valve structure, increasing the likelihood of developing mitral valve disease.
- Aging: As people age, the heart valves may undergo wear and tear, leading to calcification (hardening) of the mitral valve, making it harder for the valve to open or close properly.
- High Blood Pressure: Chronic high blood pressure puts strain on the heart and can lead to changes in the valve structure, increasing the risk of mitral valve regurgitation.
- Heart Attack: A heart attack can damage the area of the heart muscle that supports the mitral valve, potentially leading to mitral valve regurgitation.
Symptoms to Watch For:
The symptoms of mitral valve disease can vary greatly depending on the severity and progression of the condition. Common symptoms include:
- Shortness of Breath: Often worsens with physical activity or when lying down, due to fluid buildup in the lungs.
- Fatigue: Reduced blood flow and heart efficiency can lead to persistent tiredness and lack of energy.
- Chest Pain: Some people experience chest discomfort or tightness, especially during physical activity.
- Irregular Heartbeat (Arrhythmia): A common symptom, arrhythmias can cause palpitations or a fluttering sensation in the chest.
- Persistent Cough: Often a result of fluid backup in the lungs, particularly at night.
- Swelling in the Legs and Feet: As the heart struggles to pump effectively, fluid can accumulate in the lower extremities, causing noticeable swelling.
How Mitral Valve Disease is Diagnosed:
To accurately diagnose mitral valve disease, doctors may recommend several tests:
- Physical Exam: A healthcare provider listens for a heart murmur or unusual sounds, which may indicate issues with the mitral valve.
- Electrocardiogram (EKG): This test records the electrical activity of the heart, helping detect irregular rhythms and potential heart muscle strain.
- Echocardiogram: An ultrasound of the heart, this imaging test provides a detailed view of the heart’s structure and the functioning of the mitral valve.
- Chest X-ray: Allows doctors to see if the heart is enlarged or if there is any fluid buildup in the lungs.
- Cardiac Catheterization: In certain cases, a catheterization procedure may be needed to measure the pressures inside the heart chambers and assess blood flow.
Treatment Options:
The treatment for mitral valve disease largely depends on its severity and impact on a patient’s quality of life. Here are some common approaches:
- Lifestyle Changes: Mild cases may benefit from lifestyle modifications such as reducing salt intake, managing stress, and engaging in low-impact physical activity to support heart health.
- Medication: For managing symptoms, doctors may prescribe medications like diuretics to reduce fluid buildup, blood thinners to prevent blood clots, and beta-blockers to control heart rate.
- Surgery: In more severe cases, surgical intervention may be necessary to repair or replace the damaged mitral valve. Procedures include:
- Mitral Valve Repair: Often the preferred option, repair techniques involve reshaping or reinforcing the valve to restore proper function.
- Mitral Valve Replacement: If the valve is too damaged to be repaired, it may need to be replaced with a mechanical or biological valve.
- Transcatheter Mitral Valve Repair (TMVR): For some high-risk patients, a less invasive procedure called TMVR may be available, which repairs the valve without open-heart surgery.
Conclusion:
Mitral valve disease is a serious yet treatable condition. Recognizing early symptoms and seeking prompt medical care can greatly improve outcomes. Treatment options are diverse, ranging from medication to lifestyle adjustments and even surgery. By working closely with a healthcare provider, individuals with mitral valve disease can manage their condition effectively and improve their quality of life. Regular check-ups and following medical advice are essential steps in preventing complications and maintaining heart health.
.
For More Information Click here