Drug-Resistant Tuberculosis: Types, Causes, and Treatment Options
Introduction
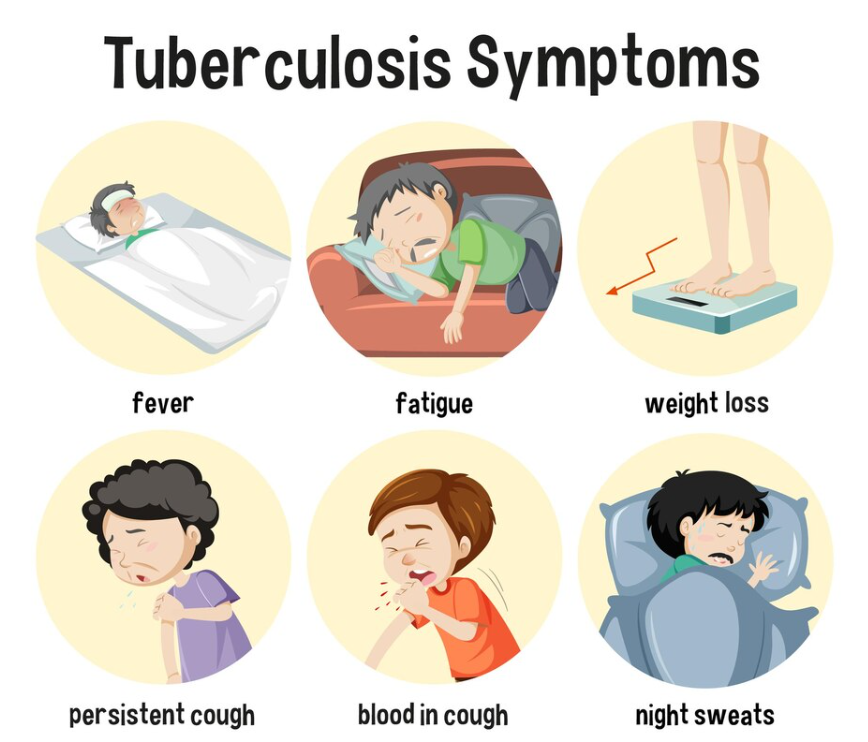
Tuberculosis (TB) is a bacterial infection treatable with antibiotics, but some TB strains are resistant to common medications. Drug-resistant TB (DR-TB) is challenging to treat and requires specialized care. In this post, we will explore the types, causes, and treatment options for drug-resistant tuberculosis.
Types of Drug-Resistant Tuberculosis
1. Multidrug-Resistant TB (MDR-TB)
MDR-TB is resistant to two of the most effective first-line antibiotics, isoniazid and rifampicin. Treating MDR-TB requires a longer and more complex treatment regimen, which may involve second-line drugs.
2. Extensively Drug-Resistant TB (XDR-TB)
XDR-TB is resistant to isoniazid and rifampicin, as well as fluoroquinolones and at least one of the injectable second-line drugs (amikacin, kanamycin, or capreomycin). This form of TB is harder to treat and has a higher mortality rate.
Causes of Drug-Resistant Tuberculosis
Drug-resistant TB develops primarily due to:
1. Incomplete Treatment
Not completing the full course of TB treatment allows bacteria to survive and develop resistance to the antibiotics being used.
2. Inappropriate Use of Antibiotics
Incorrect prescribing practices or the use of substandard or counterfeit medications contribute to the emergence of drug-resistant TB strains.
3. Inadequate TB Control Measures
Poor infection control in healthcare settings or communities can facilitate the spread of drug-resistant TB, making it harder to manage and prevent.
Treatment Options for Drug-Resistant Tuberculosis
Treating drug-resistant TB requires second-line antibiotics, which tend to be less effective and have more side effects than first-line drugs. Treatment strategies may include:
1. Second-Line Antibiotics
Drugs such as fluoroquinolones and injectable agents (e.g., amikacin) are used to treat drug-resistant TB. These are often less effective and come with more severe side effects.
2. Individualized Treatment Plans
Treatment plans for drug-resistant TB are tailored to the individual based on the specific drug resistance patterns identified through laboratory testing.
3. Directly Observed Therapy (DOT)
DOT involves healthcare professionals directly observing patients to ensure they follow the complex drug regimen. This approach helps improve adherence to treatment.
4. Supportive Care
Patients with drug-resistant TB may require additional supportive care to manage treatment side effects and complications. This can include nutritional support, pain management, and mental health care.
Conclusion
Drug-resistant tuberculosis poses a significant challenge to global health. Prevention through proper TB management and adherence to treatment protocols is essential in reducing the spread of drug-resistant TB. By addressing the causes and improving treatment options, we can work towards eliminating this global health threat.
To seek medical advice, always consult a Doctor.
Here are our recommended experts. Click here
To read more on Respiratory disease . Click Here


